
MRSA, or methicillin-resistant Staphylococcus aureus, is a superbug that you may have heard of. MRSA symptoms can include swelling and irritation of the skin. Although this superbug might not sound too serious at first glance, it’s a bacterium that resists most of the antibiotics out there. So not only is it extremely uncomfortable, it’s also incredibly difficult to treat.
This is why it’s so important to recognize the illness and get to a doctor as soon as possible. Even if you don’t have MRSA, there’s still a chance you’re a carrier for the bug, so prevention is key for literally all of us.
If you’re unsure of what to look for, we’ve put together a list of all the MRSA symptoms and signs to keep an eye out for. Plus, we’ve provided some key tips for prevention and treatment.
What Are the Different Types of MRSA?

There are two main types of MRSA strains: HA-MRSA and CA-MRSA. The main difference between the two strains is that they produce different sets of toxins and have different methicillin resistance gene cassettes. These cassettes are basically carriers for antibiotic resistance genes. Essentially, they resist different natural antibodies and medications and cause different symptoms.
HA-MRSA, or healthcare- or hospital-acquired MRSA, is more widely associated with being contracted in medical facilities. CA-MRSA, otherwise known as community-acquired MRSA, is more likely to be contracted via physical contact in daily life.
In terms of MRSA symptoms, HA-MRSA is known to cause more serious issues, such as:
- Pneumonia
- Sepsis
- Urinary tract infections
- Fevers
- Chest Pain
- Shortness of breath
- Rashes
CA-MRSA symptoms are often more skin-related, such as:
- Rashes
- Increased body hair
- Swollen lumps
- Cellulitis
How Is MRSA Contracted?

CA-MRSA is contracted through personal contact via infected wounds, rashes, razors, unwashed items of clothing, or any skin-to-skin or item-to-skin contact. So if your friend has it, and you help apply aloe cream to your friend’s mystery rash, then you might catch it yourself.
Similarly, HA-MRSA is also transferred through personal contact; however, since it’s typically contracted in a medical setting, it’s mainly contracted via surgical equipment and other medical apparatuses.
Who Gets MRSA?

Those with weak immune systems and the elderly are most likely to contract the superbug.
Evidence shows that certain ethnic groups are more likely to contract the bug than others.
MRSA Symptoms
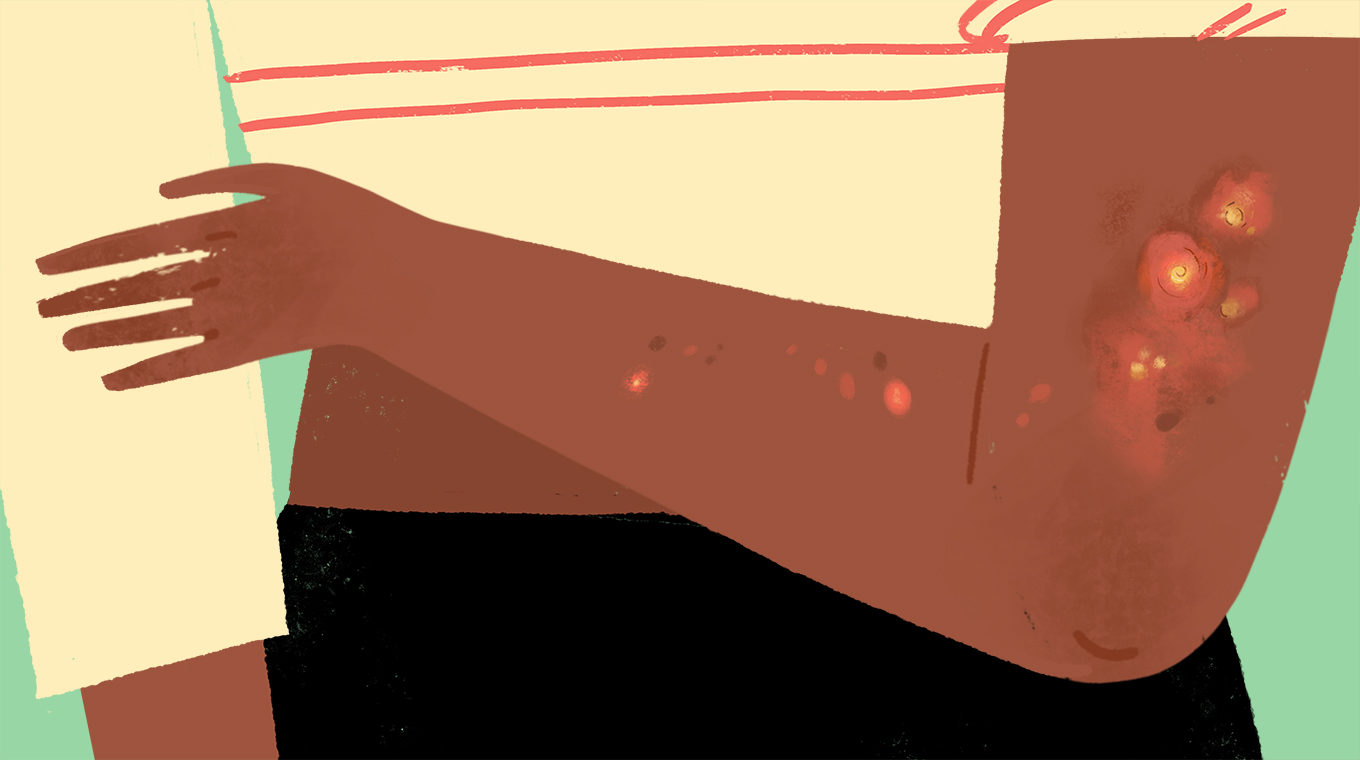
1. Red Bumps and Sores
The most recognizable MRSA symptom is bumps on the skin. The bumpy rash caused by the superbug can often look similar to chicken pox, acne, or even eczema. The bumps are usually tender, sore, and very itchy.
The lumps that look more like sores and wounds can easily be mistaken for spider bites and blisters, so whatever the rashes look like, see a doctor.
2. Cellulitis
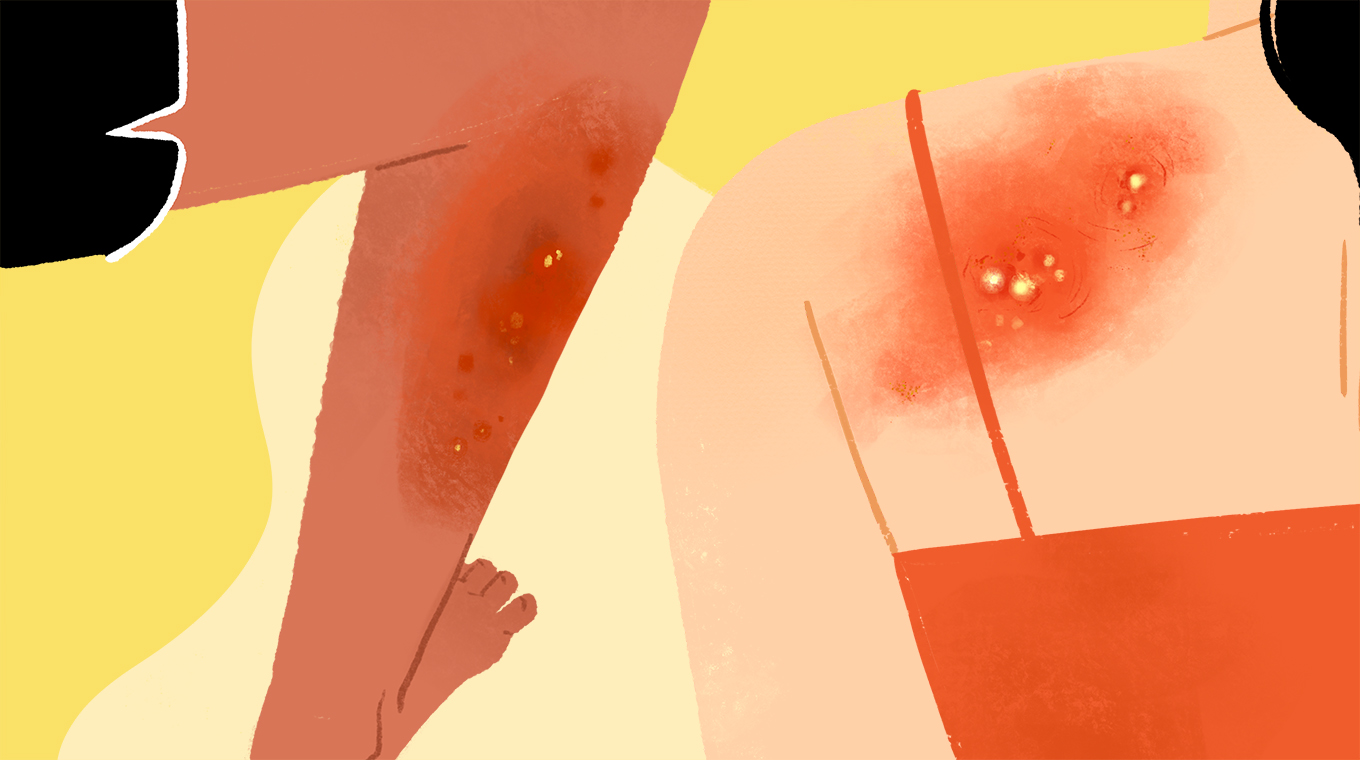
Cellulitis is an infection of the deeper layers of skin, causing the flesh area to swell. So even if the first layer of skin looks OK, an infection could be hiding deep down.
The infection basically looks like a sunburn that has taken a more serious and painful turn, and it spreads quickly. The hands, feet, arms, and legs are most often affected.
3. Fever

Like many infections, MRSA can cause a high fever. If you’re at the fever stage of the illness, then it’s a sign that any medication you’ve taken just isn’t working. This could be the stage when a doctor admits you to the hospital.
4. Warm, Itchy Skin

Alongside bumps and sores, MRSA symptoms can include warm, itchy skin. The blood rushing to the infected area increases the temperature of the skin, as does constant scratching.
As uncomfortable as it is, try not to scratch. On top of antibiotics, your doctor will also prescribe a medicated cream or ointment to deal with the itch.
5. Pus
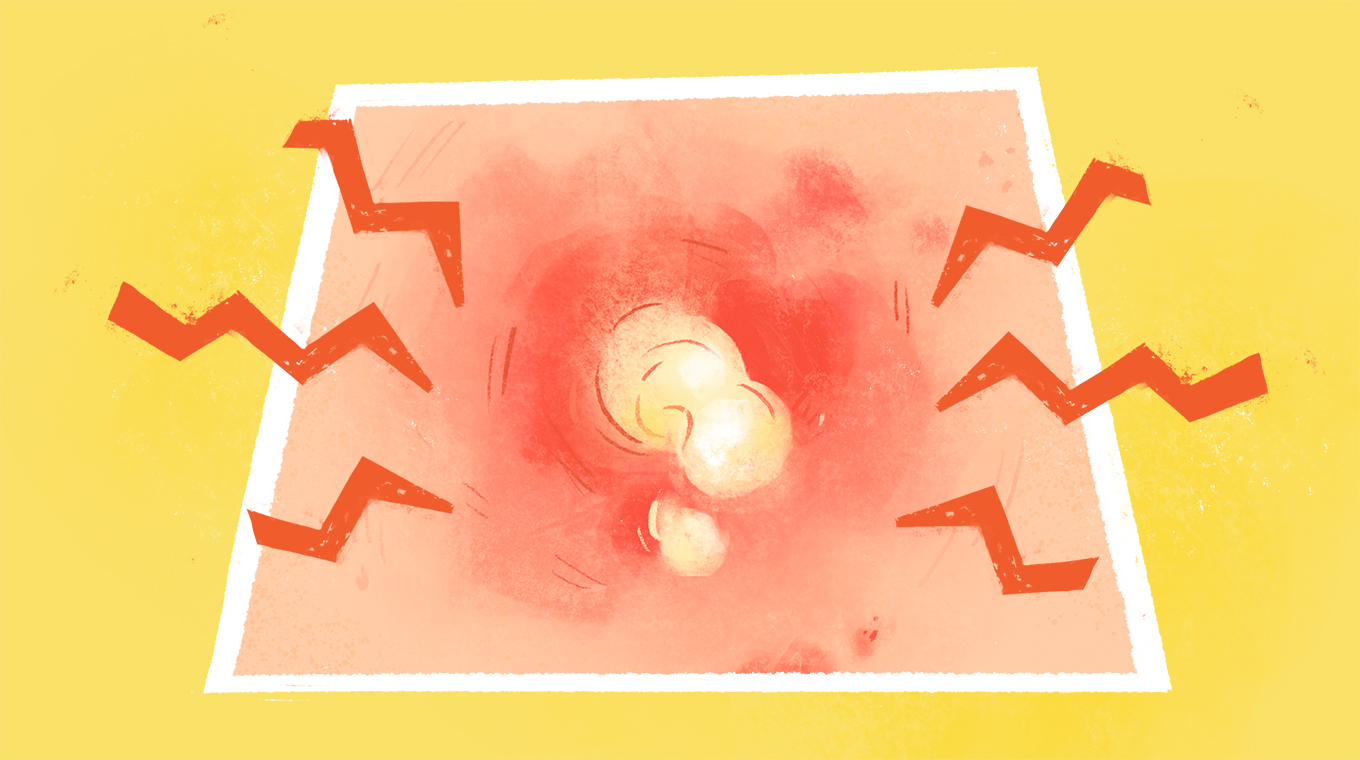
Any infected bumps, pimples, or sores will weep pus now and again, but with MRSA, there’s a lot of pus. On top of this, folliculitis (infected hair follicles) will often arise.
Just like with scratching the rashes, the urge to pop the pus pods will be strong, as will the urge to pull out the hairs stuck in the middle. But both could lead to the infection getting worse and spreading to other patches of skin.
What To Do If You Think You Have MRSA

With any scary MRSA symptoms, your first priority is not to panic. The second priority is to call your doctor and book an appointment. In the meantime, take note of all the MRSA symptoms and sensations your body is experiencing.
Also, be sure to think back to how you might have contracted it. Did you recently have a long hospital stay? Did you take a dip in a hot tub with friends? Do you remember hugging an itchy kid? Did you help wrap a bandage around your partner’s wound? Asking yourself questions like this can help you find the root of the infection and help warn those around you that they might also be infected.
Avoiding the spread of the infection is also paramount. Cover your rashes and wounds, try not to touch anyone while undergoing initial treatment, wash everything, and try to avoid community activities that are physical, such as sports and dancing.
MRSA Treatments

Part of the reason why MRSA is such a serious and difficult illness is that it resists a lot of the regular antibiotics available. So, treatment can be a little complicated for many patients.
Trimethoprim, clindamycin, sulfamethoxazole, and rifampin are some of the antibiotics widely used to treat MRSA, as they have a better track record for recovery than amoxicillin and penicillin. Mupirocin cream may also help soothe infected rashes.
General painkillers and soothing treatments such as heat packs and ice packs are always useful, too.
MRSA Prevention

Preventing MRSA is a mix of luck and common sense. Washing your skin, clothes, and swimsuits regularly is the first step, as is avoiding contact with the rashes and wounds of others. Covering your own wounds is also vital.
Oh, and be sure to clean your phone regularly, too!
Then again, sometimes you might come in contact with someone you have no idea has the bug. You could hold someone’s hand on a blind date, not knowing that person has a rash on that arm. The person might not know what it is and assume it’s just eczema.
But the risk of that isn’t too likely, so just keep clean and carry on.
1. Wash Your Hands and Clothes — A Lot

Again, it’s common sense, but we all have those times when we don’t wash our hands as well as we should.
If you aren’t sure about the cleanliness of your hands, then carry a bottle of hand sanitizer with you.
In terms of clothes, just try to avoid squeezing “one more wear” out of your favorite jeans before you wash them; it’s just not worth it.
2. Cover Any and All Wounds

This is pretty much a no-brainer, as no one really likes to walk around with open wounds. Obviously, your wounds need to meet the air now and again to be able to heal, but if you’re going outside or in physical contact with someone, get that cut covered.
Once the wound has stopped bleeding, take the bandages off when you’re alone and aren’t touching anything that could carry infection.
When To See a Doctor

Like any illness or cluster of random symptoms, you’ll always be better off going to your doctor for a diagnosis if you are experiencing any MRSA symptoms. It’s better to go and discover you just have a hay fever rash than to stay at home and soon realize you’re deathly ill.
You’re not wasting the doctor’s time, and you might actually be saving your life.
Be sure to tell the doctor everything — your symptoms, what you’ve been up to lately (contact sports, swimming, etc.), and how much pain you’re suffering from. And if the symptoms persist, go back for more care.
*Psst: if you choose to purchase an item from this post, CafeMom.com may receive a small cut. Each item and price is up to date at the time of publication; however, an item may be sold out or the price may be different at a later date.




