While it’s certainly a good thing that we ladies don’t have to resort to the birth control methods we once did, it can still be difficult to find a method that is ideal for our bodies and circumstances.
I started taking the pill when I was 16 to make my periods a bit more bearable. I loved having minor cramping instead of severe pain that made me vomit and even hallucinate. But it was annoying to remember to have to take the pill every night and refill my prescription every month. Because I’m forgetful (and yes, a bit lazy), I’ve been on and off the pill for a few years now.
After a particularly painful menstrual cycle, though, I knew I had to explore other options if I didn’t want to feel like I was on the verge of death once a month.
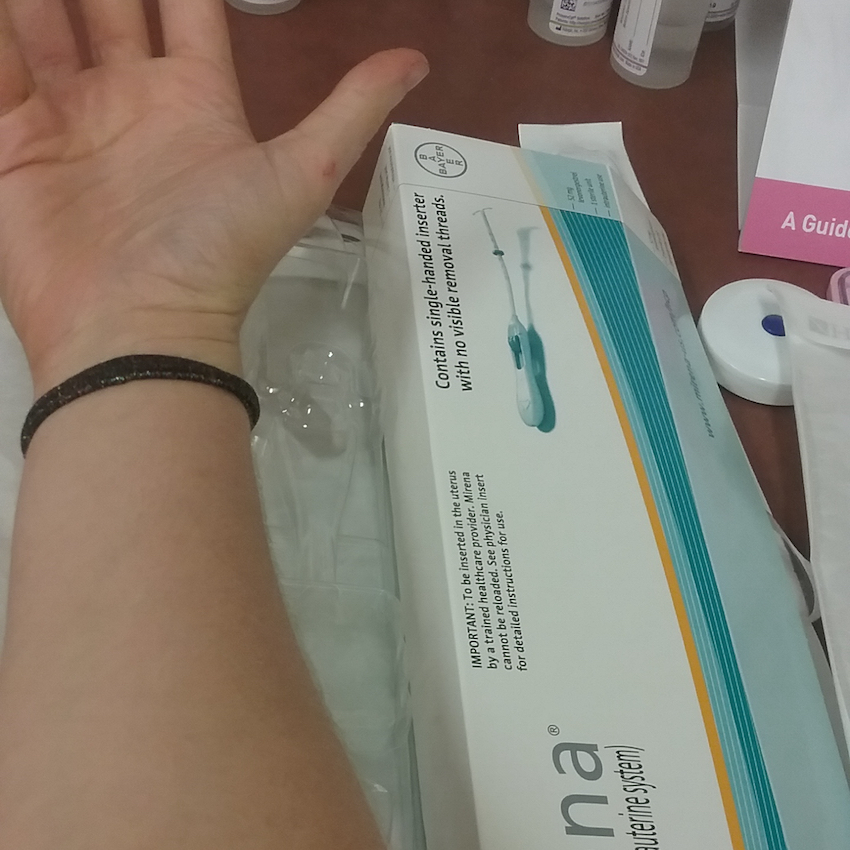
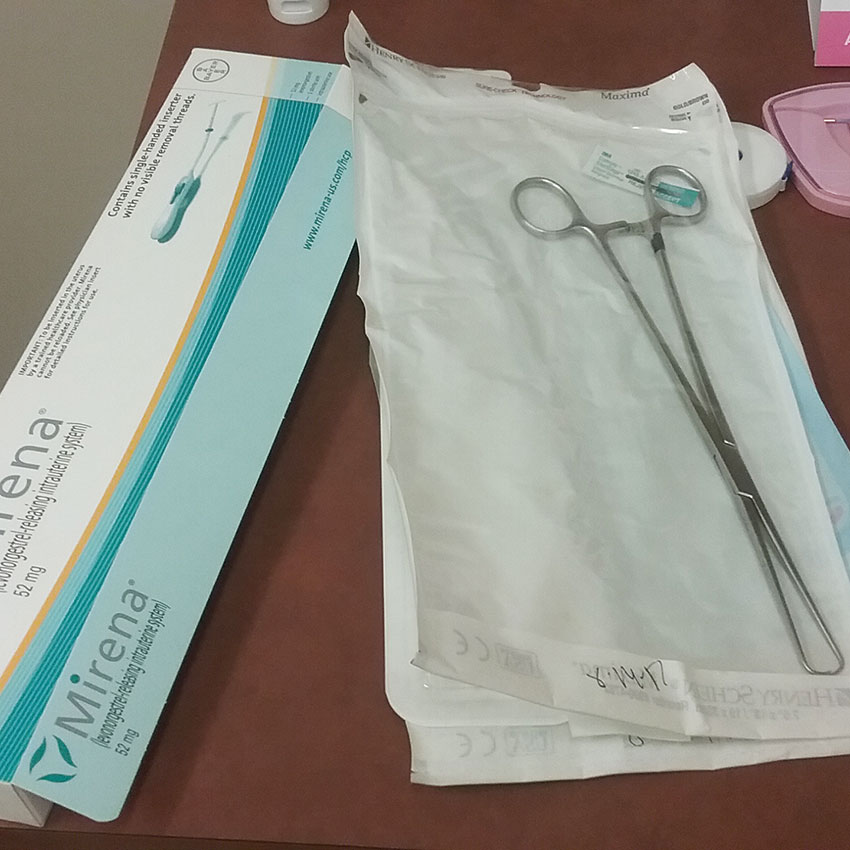
I discussed my concerns with my OB-GYN, who did a great job telling me about all the different types of long-term hormonal birth control. After careful consideration, I settled on getting a Mirena IUD (Intrauterine Device), which would allow me to not have to worry about getting pregnant or (hopefully) suffering agonizing pain during my period for the next five years.
What Is An IUD And How Does It Work?
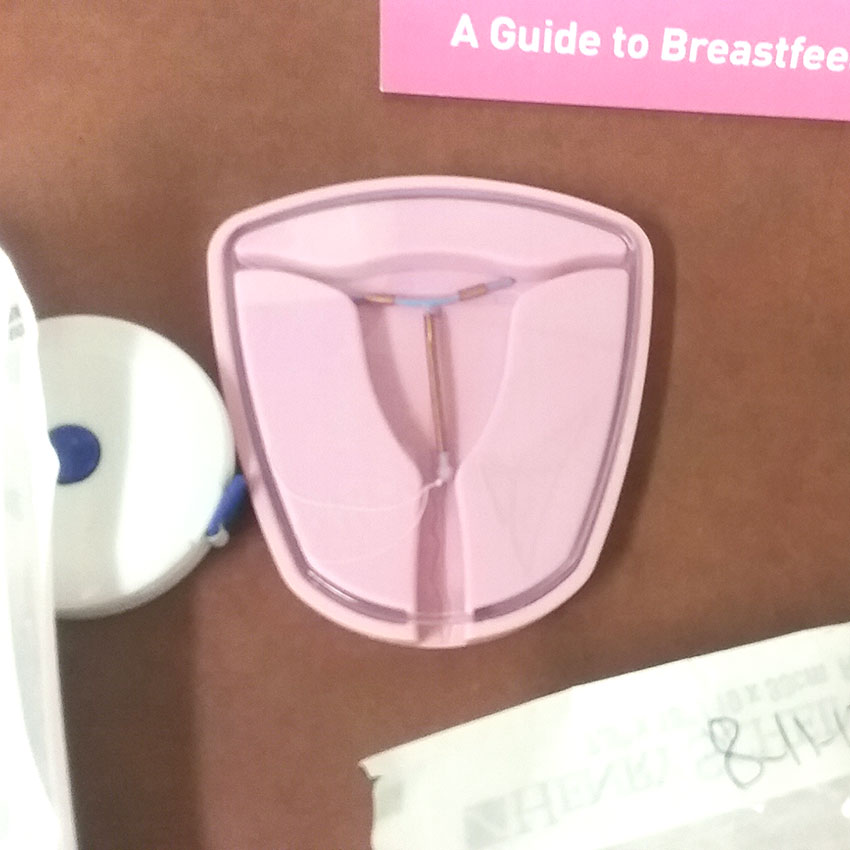
An IUD is a T-shaped device that gets inserted into your uterus. However, there are two types, and they both work differently.
The first type is a copper IUD, which is commonly known as Paragard. This IUD can be effective for up to 10 years, and it doesn’t release any hormones. Its efficacy is based on the fact that copper messes with sperm movement, making it basically impossible for them to reach and fertilize your eggs.
The second type of IUD, which includes Mirena and Skyla, is hormone-based and is generally effective for three years (for Skyla) or up to five years (for Mirena). According to the Department of Health and Human Services, this device releases a small amount of the hormone progestin, which thins the uterine lining and also makes cervical mucus thicker, causing it to act as a barrier for sperm so it can’t enter the uterus.
Both types of IUD are removable, and if you decide you do want to have kids, you can start trying to get pregnant immediately after getting the device taken out. But until that day comes, you get birth control that’s 99% effective — meaning it works even better than condoms or the pill.
Because one of my primary reasons for getting an IUD in the first place was to make my periods a bit easier on me, I opted for Mirena, since Paragard’s non-hormonal nature meant that it likely wouldn’t affect my cycle at all.
The Side Effects And Risks Of An IUD
As with any medical procedure, getting an IUD can (and frequently does) come with side effects. Some of them are beneficial — according to the Mayo Clinic, progestin-based IUDs can lighten, reduce the frequency of, or even stop your period entirely.
Insertion can also be a painful process involving severe cramps, nausea, or dizziness, but those symptoms normally go away within 30 minutes after the procedure unless the device wasn’t inserted properly.
For the first three to six months, it’s also possible to have periods that are irregular or heavier than normal while your body gets used to the IUD. In rare cases, infection can occur if bacteria gets into the uterus during the insertion process, but a good OB-GYN will take the appropriate measures to prevent this from happening.
There’s also a very small chance that the device can perforate the uterine wall, but again, this is extremely unlikely.
How Much Does It Cost To Get An IUD?

My doctor’s office checked with my insurance company to see how much I’d have to pay, and thankfully, mine was completely covered. The Affordable Care Act generally covers all or most costs for an IUD, but if you don’t have insurance, it can be pricey — up to $1,000.
However, there are other options to minimize or eliminate your out-of-pocket costs. Bayer’s ARCH (Access and Resources in Contraceptive Health) Patient Assistance Program helps pay for contraception for low-income women in the United States, and you can also see if your employer offers a health savings account (HSA) for employees with high-deductible insurance plans.
Before The Procedure
One thing I was told before I made my appointment was to try to schedule it as close to when my period started as possible to ensure that the likelihood of me being pregnant was as low as it could be. My period finished up the day before my appointment, but the nurse practitioner who performed the procedure told me beforehand that the IUD could also be inserted up to 14 days after my period started.
When I arrived for my appointment, the nurse checked my weight and blood pressure. One thing I was not expecting, however, was that they’d take a urine sample to make super-sure that I wasn’t already pregnant. I’d peed before I left the house, so it took some serious effort to force some extra urine out. If you’re going to get an IUD, go in with at least a partially full bladder so you don’t have to waste an extra five minutes in the bathroom like I did.
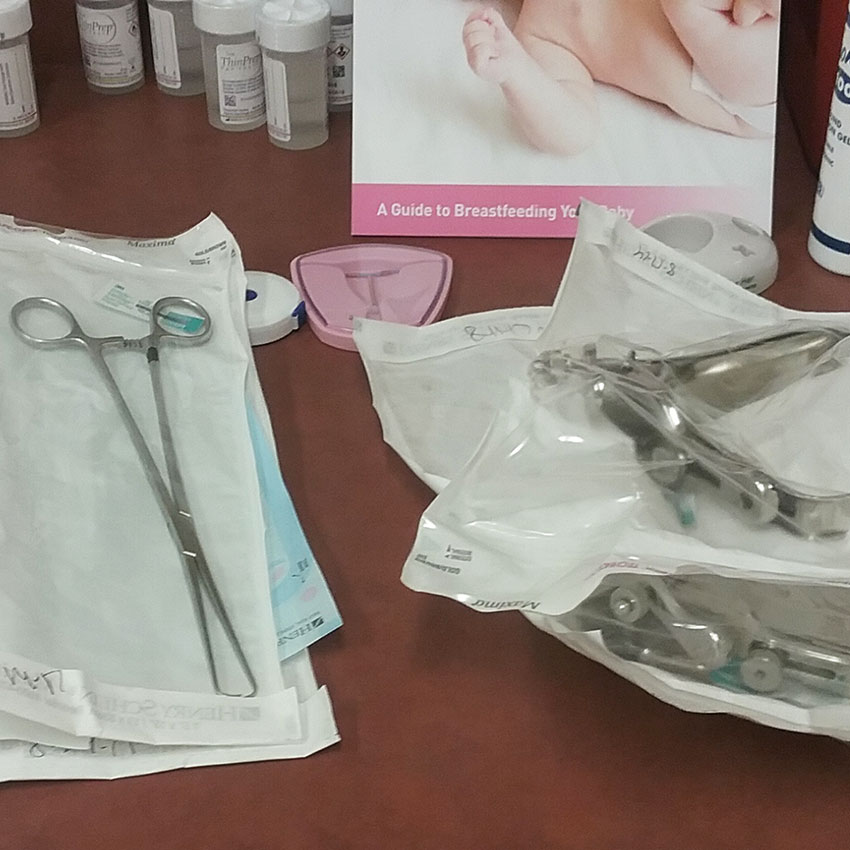
Once that was all finished, I went into the exam room and checked out all the tools. I was pretty surprised at how long everything was. The IUD insertion tool was about as long as the distance from my elbow to my fingertips.
There was also a huge pincer-like tool (that I soon discovered was called a tenaculum) that didn’t look like it was intended for anything fun, and the cotton swabs for the betadine looked like Q-tips for giants. It made sense, given the how much of my body these tools had to go through to get the IUD where it needed to be, but seeing all the large devices needed to insert such a tiny “T” caught me off guard.

I undressed from the waist down, and chilled out with the paper sheet draped over my lower half until the nurse practitioner came in.
How The Procedure Felt
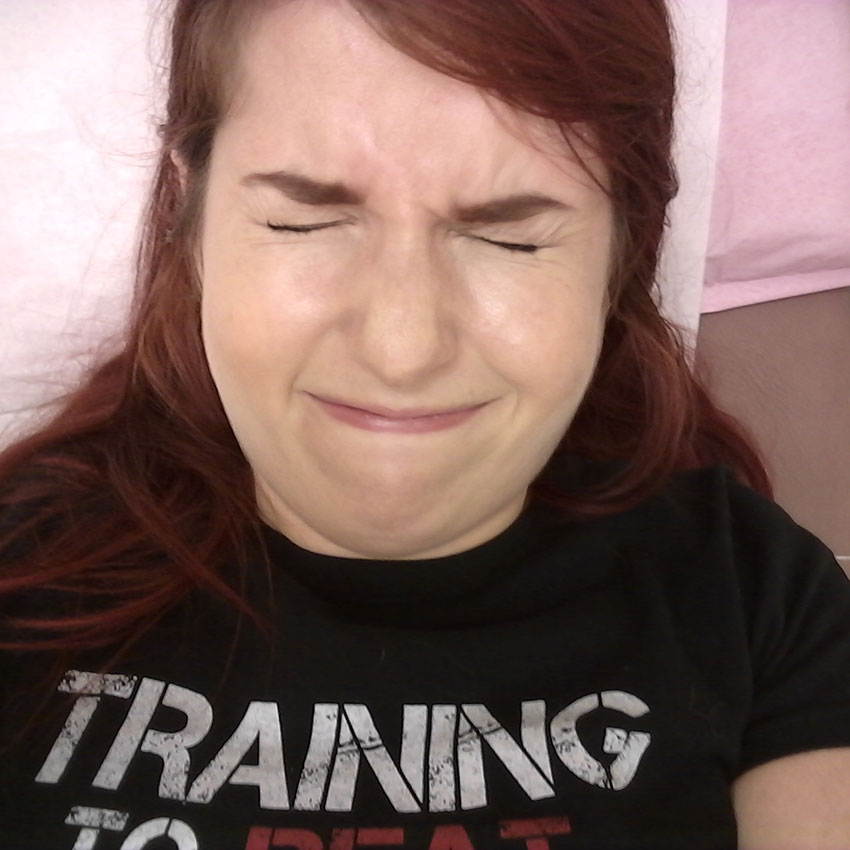
I knew going in that the IUD insertion was going to be painful, but I have a pretty high pain tolerance (especially after 16 years’ worth of torturous periods every month), so I thought I’d impress the nurse practitioner with how tough and stoic I was throughout the whole thing. I was wrong.
At my request, she explained each step of the process to me. First, she inserted a speculum, which is pretty standard procedure for anyone who’s ever gotten a pap smear — it’s not painful, but there is a bit of pressure, which can be slightly uncomfortable.
Next, she swabbed the inside of my cervix with betadine to sterilize the area, which again, felt a little weird, but didn’t hurt.
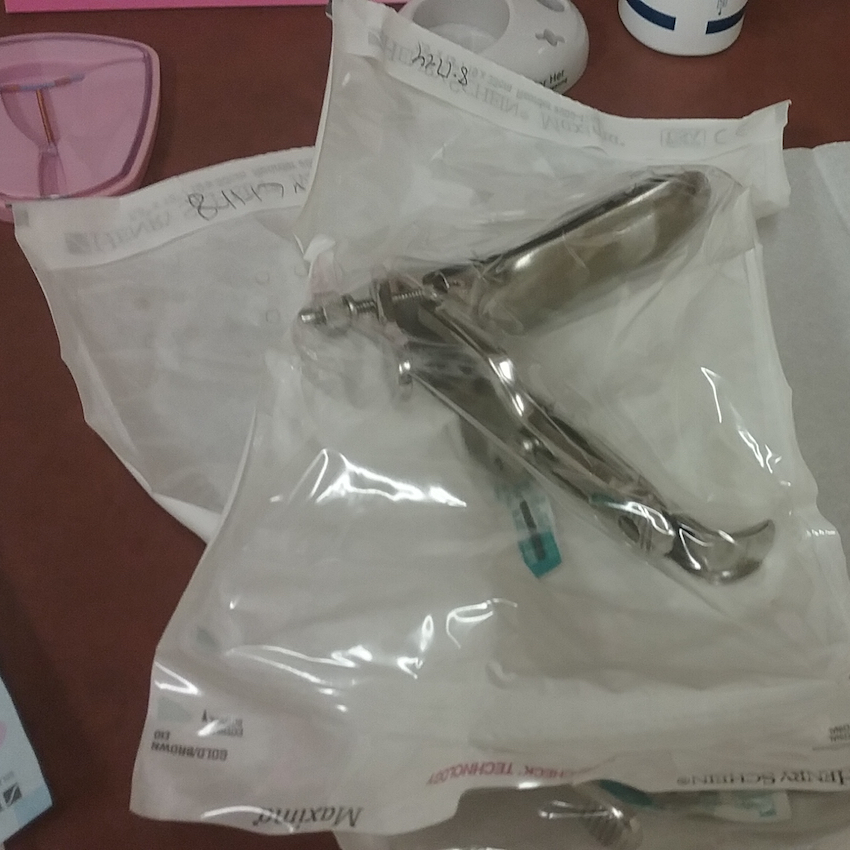
Then came the fun part: the tenaculum. That giant pincer tool that had caused me to raise an eyebrow when I first entered the room was used to clamp onto my uterus and hold it in place. This was the most painful part of the procedure. I was warned that I’d feel a little pinch, but it was actually a pretty big pinch — not surprising given that a metal instrument was clamping onto one of my organs.
From there, I started to get what basically felt like bad menstrual cramps, plus that pinching feeling of the tenaculum on my uterus. I was tensing up pretty hard, so the NP told me to take some deep breaths to help my cervix muscles relax.
But after that, the IUD was inserted within a minute, the tenaculum was removed, and the pain was gone pretty much instantly. The NP trimmed the strings attached to the IUD, which can be used to check to ensure the device is in place, and that was that.
The whole procedure took about 10 minutes, and the pain only lasted for about three.
After The Procedure
Immediately after the device was inserted, the NP said that I looked a little sick. I was slightly dizzy and nauseous, but I think it was more psychological than anything — my body is so used to throwing up when I get my period that when that pain in my uterus hit me, its natural response was to encourage me to puke.
Plus, for some reason, the sensation and mental image of that tenaculum clamping my uterus really freaked me out, and I think that made it a bit worse. I was told that there would be some bleeding afterward, so the NP gave me a thick menstrual pad to catch the blood, told me to take as long as I needed if I was feeling sick or dizzy, and then left me alone to get changed.
I still felt some very light cramping, but it was more uncomfortable than painful — almost like I just needed to use the bathroom.
In the hours that followed the procedure, there was a significant amount of blood — like the first or second day of a heavy period — but the cramping that usually comes with that level of bleeding didn’t accompany it this time.
Everyone has different experiences with degrees of pain, dizziness, nausea, and bleeding, though, so if you have a low pain tolerance, it might be a good idea to take some Tylenol or ibuprofen before you go in.
What I Wish I Had Known Beforehand
I thought I was doing the right thing by peeing before I went in for my appointment, but clearly I was wrong. Doing a urine test on a freshly emptied bladder was a challenge, but not really a huge deal.
I went into the procedure pretty well-educated thanks to the internet and my nurse practitioner being awesome about telling me everything I needed to know. However, if I had to do it over (and hadn’t needed to write this article), I probably wouldn’t have asked for the step-by-step walkthrough that she gave me.
I had thought that the pain people experienced was from the actual insertion of the device, but it’s really from the tenaculum, which again, really freaked me out for some reason. “You’re going to feel a pinch” sounds a lot more pleasantly vague than “You’re going to feel a pinch because I’m going to clamp the tenaculum onto your uterus,” but, hey, I got what I asked for.
My Final Thoughts

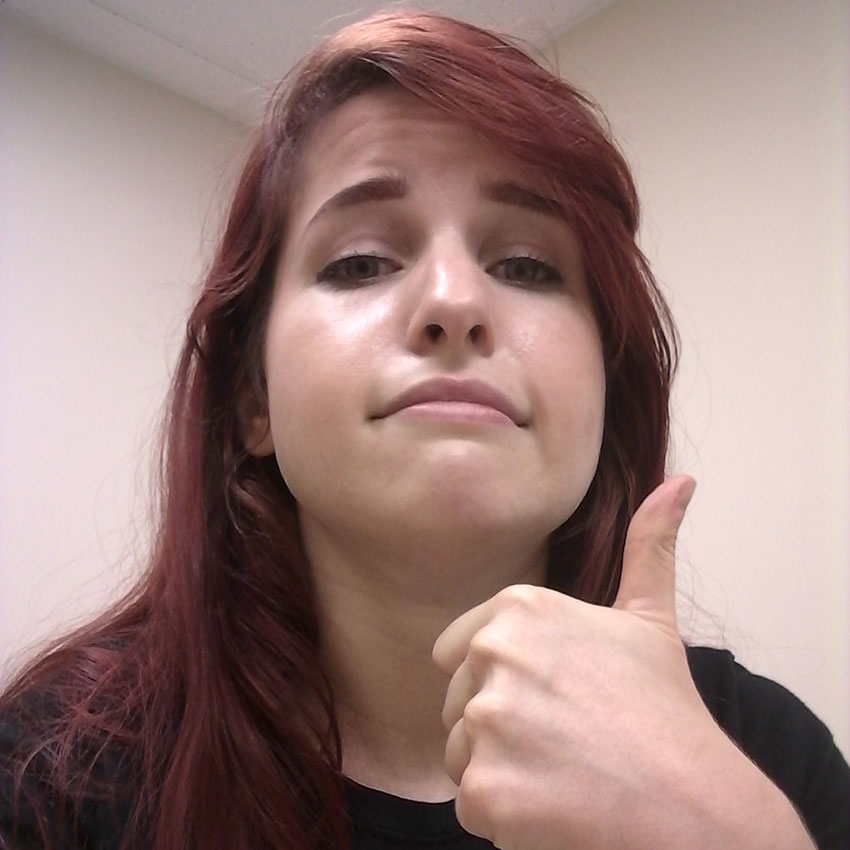
Was it worth it? The three minutes of pain I went through to have lighter periods and not have to worry about getting pregnant for the next five years was definitely worth it.
The worst part is that I’m now hyper-aware of where my uterus is. When I get cramps, it just feels like my whole abdomen hurts, but getting your uterus pinched with a metal object really has a way of making you go, “Ah, that’s where that is.” The feeling and mental image of that thing clamping down on me still makes me cringe, but luckily, I have five years to get over it.
Would I recommend it to a friend? I’d still really recommend getting an IUD if you don’t want to get pregnant in the near future or want lighter periods.
Don’t let the pain scare you away. Even knowing what I know now, it’s better than taking the risk of getting pregnant or dealing with my typically awful cramps once a month.
If you found my experience helpful, make sure to SHARE it for anyone else curious about IUDs.




